บทความ
Abstract
The aim of this study is to investigate the oral health status of dental patients with dementia and to evaluate the ability of caregivers of patients with dementia in primary oral health assessment using the Oral Health Assessment Tool (OHAT) and dysphagia detection using the Eating Assessment Tool (EAT-10). Nine dementia patients with their caregivers were voluntarily gave consented to participate in the study. Their oral health status and tongue pressure were recorded by oral examination and tongue pressure sensor device. Socio-demographic data, individual information, primary oral health assessment, OHAT, EAT-10, and any symptom-sign correlation of dysphagia were derived from an interview with caregivers. Descriptive statistics were reported by the mean with SD and percentage. The mean age of participants was 83.33 (±4.15) years old. The average remaining teeth was 11.22 (±9.74). Seven participants (77.8 %) had fixed and/or removable dental substitution. Only 33.3 % had at least 20 functional teeth, while 22.2 % had at least four posterior occluding pairs. Almost half of the participants (44.4 %) had periodontal disease, and two (22.2 %) had active dental caries. For the tongue pressure value, four (44.4 %) had a substandard tongue pressure value (less than 20 kPa) which implied the risk of dysphagia. While three out of these four cases can be detected for dysphagia signs by their caregivers using EAT-10. For the OHAT assessment, 55.6 % of the caregivers had similar OHAT scores with dental professionals. The differences between caregivers and dental professionals in their OHAT assessment were in the sections of oral cleanliness, the status of natural teeth, and the quantity of saliva, while the largest frequency of agreements were lips, dentures, and dental pain. The results showed that the oral health of the patients with dementia is not so good as almost half of the participants have a problem with periodontal disease and 70% have less than 20 natural teeth. Also almost 80 % have less than four occluding pairs. However, caregivers have the potential in dysphagia early detection and the ability in oral health assessment which indicate the need for further study and to develop a training program for caregivers.
Keywords: Caregiver, Dementia, Dysphagia, OHAT, Oral health status
Correspondence to: Orapin Komin, Department of Prosthodontics, Faculty of Dentistry, Chulalongkorn University 34 Henri-Dunant Road, Wangmai, Pathumwan, Bangkok, 10330, Thailand Tel: 02-218-8532 Fax: 02-218-8534 E-mail: Orapin.geriatric@gmail.com
Introduction
Dementia is one of the primary diseases of aging, is known as a slow, progressive, chronic decline in intellectual abilities that includes an impairment in memory, judgment, or other thinking skills which are severe enough to reduce a person's ability to perform everyday activities. Globally, 1 % of the cases appear by the age of 60 and more than 40 % of the cases occur by the age of 85.1,2 Meanwhile, in Thailand, the prevalence of dementia was reported around 3.1 to 3.4 % among older Thai people.3,4
The activities in daily living of dementia patients are not only challenging because of their dependency on their caregivers but also the provision of regular oral hygiene care with their reduced physical dexterity, impaired sensory functions, communication and behavior problems that decreases their self-care ability.5 Moreover, multiple factors in the general aging process can also lead to the cause of oral health problems such as systemic diseases and medications. Especially in older people who are cognitively impaired, they tend to have a higher risk of root and coronal caries, with more retained roots and plaque accumulation when compared to older people without dementia.6,7 This leads to many oral health problems related to oral soft tissues such as gingival bleeding, periodontal pockets, stomatitis, mucosal lesions, and hyposalivation.8 People with edentulous cognitive impairment have a tendency to have poorer denture hygiene condition than people who are cognitively healthy.9 This brings the idea that the caregivers of patients with dementia play an important role for the physical, psychological and dental conditions of their patients.
Besides oral hygiene, and oral function; chewing ability is another concern for dental care. In the oral stage, the first stage of chewing performance, teeth and tongue help in grinding foods to form a bolus. Then, the bolus will be swallowed into the gastrointestinal tract by the process of the pharyngeal and esophageal stages respectively. An estimated 45 % of institutionalized patients with dementia have dysphagia.10,11 The high prevalence of dysphagia in individuals with dementia is the result of age-related changes in sensory and motor functions. The consequences of dysphagia may be dehydration, malnutrition, weight loss, and aspiration pneumonia; a common cause of morbidity and death. Afterall, in the late stage, patients with Alzheimer may be unable to manipulate the bolus or chew adequately to meet their nutritional needs.10 Patients with moderate to severe Alzheimer’s have an especially high risk of malnutrition which is a common contributor to mortality.12,13 The Body-Mass Index (BMI) seems to be not only a good nutritional parameter but also an indicator of global health status in older people with dementia.14 A lower BMI is associated with increased mortality risk in individuals with dementia.15
For these problems, the movement of the tongue plays a crucial role in maintaining a cohesive bolus while manipulating the bolus during mastication and propelling the bolus out of the oral cavity and through the larynx in the oral-stage of swallowing. The tongue pressure sensor device is a device that measures the pressure of the tongue in kilopascal (kPa). This force will be obtained when the dorsum of the tongue touches the hard palate while the person is swallowing. The obtained pressure value has a significant relationship with the tongue muscle strength which is also related to the oral-phase swallowing function especially for bolus formation, mastication, premature bolus loss, tongue to palate contact, and oral transit time.16 The strength of the tongue needs to be maintained for proper swallowing and also when the force drops, it can be an objective indicator for monitoring dysphagia evaluation.16-18 Providently, there is a validated and reliable self-administered instrument for symptom-specific survey for dysphagia called ‘Eating Assessment Tool’ or ‘EAT-10’. This instrument may be utilized as a clinical instrument to document the primary detection in older people with dysphagia. EAT-10 is a subjective dysphagia assessment tool that helps to measure swallowing difficulties. The normative data suggest that an EAT-10 score of 3 or more is abnormal.19,20
For these reasons, caregivers are the key person in notice any signs of dysphagia and maintain oral health and hygiene of dementia older people. This could be achieved by care education for caregivers in behavior management, individualized oral health care plan, and the training in usage of simple screening tools such as Oral Health Assessment Tool (OHAT) and Eating Assessment Tool (EAT-10). It is much more benefit when the caregivers can early detect any signs and liaise with dental professionals in regular professional dental care.5,8 This also promotes a multidisciplinary approach with physicians, nurses, family members, caregivers and dental professionals sharing responsibility for the four key processes: oral health screening, oral health care planning, daily oral hygiene and access to dental treatment.21
There are still fewer studies about the relation between dementia and oral health status in Thailand.22 The authors aim to investigate the oral status of the dementia dental patients at the Faculty of Dentistry, Chulalongkorn University and to evaluate the ability of caregivers of patients with dementia in primary oral health assessment using OHAT and dysphagia detection using EAT-10. We hope this study will enable Thai dentists to understand the oral health status of patients with dementia and collect useful data for the further full-scale study and the optimal oral health care protocol or standard training program development for caregivers of patients with dementia.
Materials and Methods
This cross-sectional descriptive pilot study enrolled patients with dementia who are current dental patients at geriatric clinic of Faculty of Dentistry, Chulalongkorn University during March to May 2019 with their caregivers. Patients with dementia with their caregivers were invited after screening by the specific inclusion criteria; be diagnosed dementia, have the ability to communicate in Thai with cooperative along the study protocol. All participants’ caregivers must have the capacity to give their consent in written consent form for study participation after being thoroughly informed about the study protocol. Participation is always voluntary. The study protocol was under the approval of the Ethical committee at the Faculty of Dentistry, Chulalongkorn University (HREC-DCU 2019-006).
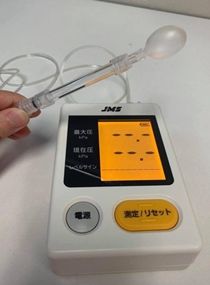
The oral health status data and current dentition of participants were collected by oral examination. Denture history were interviewed, and tongue muscle strength were measured by TP. Current dental substitution type with patient’s satisfaction, Number of natural teeth (NT) (classified into two groups; less than 20 NTs and at least 20 NT), Number of Posterior Opposing Pairs (POPs) (classified into two groups; less than 4 POPs and at least 4 POPs), Periodontal disease; the presence of at least two proximal sites of non-adjacent teeth having clinical attachment loss ≥ 3 mm will be defined as present periodontal disease,23 Present of active tooth decay, and tongue pressure by The JMS tongue pressure measurement device; Orarize® TPM-01, JMS Co.,Ltd. Hiroshima, Japan (Fig. 1). After device calibration for 20 kPa in the bulb, participants were seated up-right and asked to “press your tongue against the bulb as hard as possible”. Three trials of maximum performance will be collected and recorded. The highest score will be used for the maximum tongue pressure (Fig. 2).
Figure 1 JMS tongue pressure measurement device (Orarize® TPM-01, JMS Co.,Ltd. Hiroshima, Japan)
Figure 2 JMS tongue pressure measurement device usage
The standard tongue pressure for people age 70 year old and over from the device manual is 20 kPa.24 Socio-demographic data, individual information, primary oral health assessment, and any symptom-sign correlation of dysphagia derived from the caregivers’ interview; including age, sex, marital status, living condition, educational level, occupation defined as the longest job they have held, current income, weight, height, Body Mass Index (BMI), mini nutritional assessment (MNA) as a nutritional status, diagnosis and duration of dementia, family history of dementia, drug abuse, exercise, The Barthel Activities in Daily Living; ADL and the Lawton Instrumental Activities in Daily Living; IADL as functional assessment. For the social interaction, the cognitive training activities, the frequency of of social contact (at least 30 mins a day) or the social media using time were recorded. For the second objective, the EAT-10 was questioned to the caregivers, then used the obtained score for classified the participants into two groups by using three scores cut point as normal and at risk to dysphagia. The OHAT was used for the caregivers along with dental profession to evaluate the patient, then both obtained results were compared. While caregiver characteristics recorded in relationship to the patient as formal, informal, or family members, total experience of elderly caregiving and hours spent caregiving.
Statistical analysis was performed by using the IBM Statistics Package for the Social Sciences (SPSS) version 22.0. Descriptive statistics were reported by the mean with SD and percentage. All of the data collection procedures were completed by only one investigator.
Results
Nine participants with dementia were included with their caregivers. The mean age of the participants dementia was 83.33 (±4.15) years, while age range was 79 to 92 years old. Most were female (77.8 %), married (55.6 %), lived with their family (88.9 %), and had at least six years of formal education (77.8 %). Self- employed/business as the longest job in life and having less than 10,000 THB for monthly income were majority of study participants. Mean BMI was 22.14 (±2.41) kg/m2. Around half of participants (55.6 %) had over in waist circumference. All had been diagnosed with dementia for at least 18 months. The mean duration with dementia was 37 (±15.38) months. Seven were functionally independent according to Barthel ADL (77.8 %). Eight participants (88.9 %) went out to a social engagement at least once a week, while only five (55.6 %) had lifelong learning or cognitive training activities at least once a week. Only two (22.2 %) use social media at least once a week.
The mean of caregivers’ experience and caregiving time was 38.29 (±32.99) months and 18.00 (±7.75) hours per day, respectively. Demographic characteristics and bio-socio-economic factors results were reported as shown in Table 1.
Table 1 Demographic characteristics and Bio-socio-economic factors of patients with dementia (n = 9)
| Characteristics | Number (%) |
|---|---|
|
N = 9 (persons) |
|
|
Gender |
|
|
Marital status |
|
|
Living condition |
|
|
Education |
|
|
Occupation |
|
|
Monthly income (Baht) |
|
|
BMI (mean ± SD) |
22.14 (±2.41) |
|
Waist Circumference |
|
|
Duration of dementia (months) (mean ± SD) |
37.00 (±15.38) |
|
Dependency level according to Barthel ADL |
|
|
Lifelong learning & Cognitive training |
|
|
Social engagement |
|
|
Social media using |
|
|
*SD = Standard Deviation |
|
More than 75 % (77.8 %, seven participants) have fixed and/or removable dental substitution in acceptable conditions; The average remaining teeth was 11.22 (±9.74). Only three participants (33.3 %) had at least 20 functional teeth. Only two participants (22.2 %) had at least four posterior occluding pairs. Mean number of posterior occluding pairs was 1.11 (±1.76) pairs, which having four pairs was the maximum POPs of participants. Almost half (44.4 %) had periodontal disease, while two participants (22.2 %) had active dental caries. All of the oral health status was reported as shown in Table 2.
Table 2 Oral health status of patients with dementia (n = 9)
|
Oral health conditions |
Number (%) |
|---|---|
|
Dentition status
|
3 (33.3) 1 (11.1) 1 (11.1) 2 (22.2) 2 (22.2) |
|
Number of Natural Teeth
|
11.22 (±9.74) 0 – 23 |
|
Groups of Natural Teeth
|
6 (66.7) 3 (33.3) |
|
Number of POPs
|
1.11 (±1.76) 0 – 4 |
|
Groups of POPs
|
7 (77.8) 2 (22.2) |
|
Periodontal disease
|
5 (55.6) 4 (44.4) |
|
Active caries
|
7 (77.8) 2 (22.2) |
|
Tongue pressure (kPa)
|
23.36 (±10.96) 9.4 – 39.6 |
|
Groups of Tongue pressure
|
5 (55.6) 4 (44.4) |
|
*NT = Natural Teeth POPs = Posterior Opposing Pair(s) kPa = kilopascal |
|
Tongue pressure of these participants were various from 9.4 to 39.6 kPa, which the mean of tongue pressure was 23.36 (±10.96) kPa. Four (44.4 %) participants had sub-standard tongue pressure; less than 20 kPa which implied the risk of dysphagia. While three out of four sub-standard tongue pressure cases can be detected for dysphagia signs by their caregivers using EAT-10. More than half of the caregivers had similar OHAT scores with dental professionals. Six cases were at risk of malnutrition due to their MNA score. BMI range showed only one case having less than 18.5 kg/m2 indicated for underweight level. The tongue pressure, EAT-10 score and OHAT agreement were reported as shown in Table 3.
Table 3 Tongue pressure, EAT-10 score and OHAT score (n = 9)
|
Participant no. |
Age (years) |
Tongue pressure (kPa) |
Tongue pressure interpret |
EAT-10 score |
EAT-10 score interpret |
MNA |
MNA result |
BMI |
BMI range |
OHAT |
|---|---|---|---|---|---|---|---|---|---|---|
|
1 |
85 |
9.4 |
Abnormal |
N/A |
N/A |
8/14 |
At risk |
17.3 |
Underweight |
Agree |
|
2 |
79 |
37.5 |
Normal |
0 |
Normal |
12/14 |
Normal |
25.4 |
Obese |
Agree |
|
3 |
82 |
22.9 |
Normal |
2 |
Normal |
12/14 |
Normal |
23 |
Overweight |
Disagree |
|
4 |
81 |
31.0 |
Normal |
0 |
Normal |
N/A |
N/A |
N/A |
N/A |
Disagree |
|
5 |
92 |
10.9 |
Abnormal |
5 |
At risk |
9/14 |
At risk |
22.5 |
Normal |
Agree |
|
6 |
86 |
17.1 |
Abnormal |
5 |
At risk |
10/14 |
At risk |
21.4 |
Normal |
Agree |
|
7 |
79 |
16.6 |
Abnormal |
4 |
At risk |
11/14 |
At risk |
22.8 |
Normal |
Disagree |
|
8 |
85 |
39.6 |
Normal |
0 |
Normal |
11/14 |
At risk |
20.8 |
Normal |
Disagree |
|
9 |
81 |
25.2 |
Normal |
0 |
Normal |
11/14 |
At risk |
23.9 |
Overweight |
Agree |
|
*N/A = Not Available |
||||||||||
Eight aspects of OHAT were verified by only one investigator and caregivers including lips, tongue, gum & tissues, saliva, natural teeth, dentures, oral cleanliness, and dental pain. Each part of OHAT presents 0-2 score meanings; 0 = Healthy, 1 = Changes, and 2 = Unhealthy.
Five out of nine caregivers have similar OHAT scores with dental professionals. The differences between caregivers and dental professionals in their OHAT assessment are in the sections of oral cleanliness, the status of natural teeth, and quantity of saliva, while the largest frequency of agreements were lips, dentures, and dental pain. OHAT scores are reported as shown in Table 4.
Table 4 OHAT scores assessed by Caregiver and Dental professional (n = 9)
| Participant no. | OHAT category (Score by Caregiver / Score by Dental professional) | Caregiver total score | Dental professional total score | Agree-ment | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lips | Tongue | Gum & Tissues | Saliva | Natural teeth | Denture | Oral cleanliness | Dental pain | ||||
|
1 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0 |
0 |
Agree |
|
2 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0 |
0 |
Agree |
|
3 |
0/0 |
0/0 |
0/1 |
0/0 |
0/1 |
N/A |
0/1 |
0/0 |
0 |
2 |
Disagree |
|
4 |
0/0 |
0/1 |
0/1 |
0/1 |
0/1 |
0/0 |
0/1 |
0/0 |
0 |
3 |
Disagree |
|
5 |
0/0 |
0/0 |
0/0 |
0/0 |
N/A |
0/0 |
1/1 |
0/0 |
1 |
1 |
Agree |
|
6 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
N/A |
0/0 |
0/0 |
0 |
0 |
Agree |
|
7 |
0/0 |
1/1 |
0/0 |
0/1 |
0/1 |
N/A |
0/2 |
0/0 |
1 |
5 |
Disagree |
|
8 |
0/0 |
1/1 |
0/0 |
0/1 |
0/0 |
0/0 |
1/1 |
0/0 |
2 |
3 |
Disagree |
|
9 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0/0 |
0 |
0 |
Agree |
|
*Each part of OHAT presents 0-2 score meanings (0=Healthy, 1=Changes, and 2= Unhealthy). |
|||||||||||
Discussion
The average age of study participants is 83.33±4.15 years old, which may result in poor oral status as shown in that 70 % still have less than 20 natural teeth, also almost 80 % have less than four occluding pairs. Furthermore, almost half of the participants have a problem dealing with periodontal disease. This implied insufficient chewing performance and may affect food preferences in types and consistency decided by caregivers. Despite low-level income of most participants, more than 75 % have fixed and/or removable dental substitutions in acceptable conditions which implied for better access to oral health care, living with family support, and the urban location of the study site.
Six cases were found at risk of malnutrition according to the MNA score. This might be a result of dependency on caregivers and limited choices due to autonomy of communication, as well as the nutritional status of each meal. The nutrition gained from types of food and consistency preferences may have resulted in having more carbohydrates than protein or vitamins and minerals from vegetables and fruits. Not only the chewing performance from dentition, but the swallowing problem also represents the oral function of individuals with dementia that could affect the nutritional and global health status in the BMI and MNA results.14
In this study, the tongue pressure was obtained for an objective measurement of dysphagia signs, while EAT-10 was collected for subjective evaluation through the key person of this population who are the caregivers. The standard tongue pressure for people age 70 years old and over from the device manual is 20 kPa while the study in 2008 showed the average maximum tongue pressure 31.9 ± 8.9 kPa in the seventies.25 Three out of four participants who had sub-standard tongue pressure can be detected for dysphagia signs by their caregivers using EAT-10. Further research needs to find the relationship between the incidence of aspiration pneumonia and the weakness of tongue muscles. Moreover, five out of nine caregivers have similar OHAT scores with dental professionals. The differences between caregivers and dental professionals in their OHAT assessment were in the sections of oral cleanliness, the status of natural teeth, and quantity of saliva, while the sections they were in agreement regarding lips, dentures, and dental pain. This might be a result of the sites of each OHAT aspect during the observation period of the caregivers; the intraoral parts seem to be more complicated for the non-dental professionals. The attitude of caregivers in reaching into the oral cavity of patients with dementia might also affect the oral hygiene care in daily routine which is a crucial part for a long-term care plan.
The dysphagia risk found in 4 out of 9 cases (almost 50 %) may also be a result of the older age of this population. Unfortunately, this pilot study has no data about the severity of dementia, the history of treatment and current medications which can describe the higher risk for dysphagia especially in the late stage of patients with dementia.10 Besides, all the participants with dysphagia risk in this study need to be referred to a rehabilitation specialist for clinical diagnosis and proper treatment for their needs.
From these pilot study results, we may know where to emphasize on the caregiver training program by pointing up to personalized dental care plan and prevention. Also, it appears that this study shows the potential of the caregivers in dysphagia early detection and oral health assessment. The caregivers who can detect this symptom have more than three years of work experience. The work experience of each caregiver and the time spent with the patient are other important factors. These topics need to be considered and explored more regarding types; formal or informal, the caregiver living conditions, and the relationship between the caregivers and the dementia individuals. Based on the results it is suggested that the professionalization of the caregivers including perception and attitude towards holistic care is important, not only for oral health and dysphagia literacy but also the ability to recognize or identify the abnormal is required. Caregivers are key persons in dependent stage of the overall health and quality of life of the patient with dementia. They need to be encouraged, empowered, and prioritized for future training program development as shown in Figure 3.
The pathway of caregiving to dependent patients with dementia through oral function and oral hygiene promotion by EAT-10 and OHAT as subjective evaluation instruments.
However, this study is relatively small in size as a pilot study and so the conclusions are limited. There needs to be a focused full-scale study which should be modified for the development of training programs for caregivers especially in oral health and dysphagia signs literacy such as the use of oral health screening tools and oral care instrument and education. Furthermore, the encouragement in perceptions and attitudes of caregivers towards oral health care and the accessibility to the dental services for older people with dementia is also needs to be achieved.
Conclusions
The results showed that the oral health of patients with dementia is not so good as almost half of the participants have problems dealing with periodontal disease and 70 % still have less than 20 natural teeth also almost 80 % have less than four occluding pairs. Anyway, it is useful to know that the caregiver has the potential to help in dysphagia early detection and ability in oral health assessment which indicate the need for further study and development of a training program for caregivers.
Acknowledgement
The authors declare no conflict of interest and this pilot study is under private funding. We would like to thank all participants and their caregivers for their helpful cooperation. We appreciate the kind assistance of all the staff members s at the geriatric clinic of Faculty of Dentistry, Chulalongkorn University.